
People who follow the federal government’s guidelines on seafood consumption are likely to consume too much mercury, a dangerous neurotoxin, or too few beneficial omega-3 fatty acids, according to a new EWG analysis of fish contaminant and nutrient data.
With the January 2011 release of the 7th edition of the federal Dietary Guidelines for Americans, a massive Congressionally-mandated white paper that sets the scientific and policy basis for all government nutrition programs, officials at the departments of Health and Human Services and Agriculture encouraged Americans to more than double their consumption of seafood from 3.5 ounces to eight to 12 ounces weekly. They urged pregnant women and people at risk of heart disease to consume 1,750 milligrams a week of healthy fats known as omega-3 fatty acids that are abundant in some fish and shellfish. Relatively recent studies indicate that these fats improve the health of the eyes, heart and nervous system, lower blood cholesterol and triglyceride levels, reduce blood pressure and aid fetal and infant brain development (USDA 2010).
At the same time, federal officials warned pregnant women to limit or avoid five high-mercury species, heed bulletins that locally caught fish could be contaminated and vary the types of fish and shellfish they eat. These cautions echoed a 2004 warning, issued jointly by the federal Food and Drug Administration and Environmental Protection Agency, that aimed to reduce mercury exposure among American women who were or might become pregnant, nursing mothers and young children. Decades of industrial mercury emissions around the world have contaminated some fish and seafood, particularly larger, long-lived deep-water species.
Yet neither official document fully addressed mercury risks during pregnancy. To the contrary, if pregnant women doubled their seafood consumption to comply with the Obama administration’s Dietary Guidelines, they could run the risk of consuming harmful amounts of mercury.
EWG’s analysis of the mercury and omega-3 concentrations in seafood found that eating fish indiscriminately can be ineffective and even dangerous. Most of the commonly eaten species such as shrimp and catfish are very low in beneficial omega-3 fats. Eating more of them won’t provide high-risk groups with enough omega-3s.
As well, EWG has compiled a list of “moderate mercury” species that would pose a mercury risk for pregnant woman and children who eat fish regularly. This list is more comprehensive than the 2004 EPA/FDA advisory, which warned that women of childbearing age and young children, who are most susceptible to the damage done by mercury, should eat only six ounces a week of albacore tuna and should avoid four other high-mercury species – swordfish, tilefish, king mackerel and shark.
The Dietary Guidelines issued in 2011 (backdated to 2010) downplayed the risks of mercury and other contaminants, asserting that that the benefits of eating fish outweighed the risks of mercury toxicity, even during pregnancy (USDA 2010). This advice conflicts with several recent studies of American families that found that children born to women with slightly elevated mercury levels suffered measurable brain and nervous system deficits (Oken 2005, Oken 2008, Lederman 2008) or were more likely than average to be diagnosed with attention deficit-hyperactivity disorder (Sagiv 2012).
This month, HHS and USDA officials and a panel of scientific and medical experts from industry and academe are meeting to plan for the 2015 edition of the Dietary Guidelines. Meanwhile, on a separate policy track, officials at the EPA and FDA are updating their 2004 fish-mercury advisory, aiming to release a new draft sometime this year.
As both sets of deliberations progress, they should strive to offer Americans advice that will enable them to enjoy the benefits of seafood consumption while keeping their mercury intake to safe levels. At present, neither the 2004 EPA/FDA advisory nor the 2010 Dietary Guidelines give people what they desperately need – precise, science-based information on how to consume sufficient omega-3s while keeping mercury levels as low as possible.
Not all seafood is equally rich in omega-3s
EWG investigated mercury contamination and beneficial omega-3 levels in seafood in order to identify species that offer the greatest health benefit and lowest mercury.
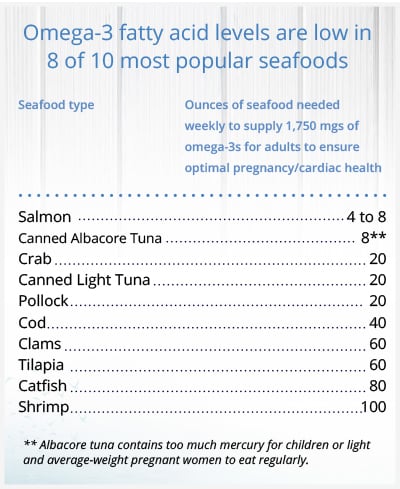
According to EWG’s calculations, eight of the 10 species that make up 90 percent of the U.S. seafood market are nearly devoid of the two omega-3 fatty acids found in other seafood – docosahexaenoic acid and eicosapentaenoic acid, often denoted as DHA and EPA. A person would have to eat between 20 and 100 ounces of those eight varieties to consume 1,750 milligrams of omega-3s weekly, the amount scientists have deemed necessary for a healthy pregnancy and for reducing the risk of heart disease. The complication and expense of eating so much fish could be prohibitive for many Americans. And if large segments of the population adopted such a fish-heavy diet, the pressure on already stressed fisheries would quickly mount to extreme and unsustainable levels.
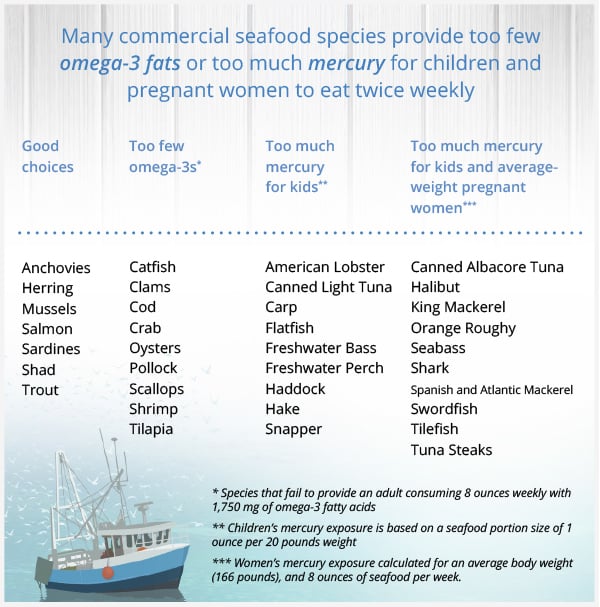
EWG calculates that 10 of 35 popular seafoods in the U.S. market would pose a mercury risk to an average-weight pregnant woman who eats eight ounces weekly, as the federal government recommended. Since safe mercury levels are based on a woman’s body weight, lighter women are more at risk from mercury in seafood. Because they are light and their bodies are still developing, children who eat 19 of the 35 popular species twice weekly face a mercury risk.
Moreover, not all fish are equally nutritious: 21 of the 35 species EWG investigated would not provide the 1,750 milligrams of omega-3 fatty acids recommended if eight or even 12 ounces of that species are consumed weekly.
Among popular seafood species, salmon stands out as an excellent choice. Four to eight ounces of salmon weekly, depending on the species, can provide 100 percent of the recommended amount of omega-3s. Some types of farmed salmon present significant environmental health concerns. EWG recommends that people choose wild salmon instead.
EWG’s analysis highlights several other affordable and sustainably produced species, including anchovies, sardines, farmed trout, and mussels. Just four to eight ounces of these species weekly would meet recommended omega-3 requirements for pregnant women and people with heart disease.
EWG’s review of mercury and omega-3 fatty acid levels found dramatic differences among species that present an opportunity for solid, practical guidance for consumers. The chart below presents a general analysis of available data of mercury and omega-3 concentrations for 35 common species. To make the very best dietary choices, consumers should also take into account recommendations for portion size and frequency. These depend on an individual’s age, weight, pregnancy status and risk of heart disease. EWG’s table is a starting point and does not reflect differences among regions or sub-species in mercury contamination or omega-3 concentrations.
When the federal Dietary Guidelines and EPA/FDA fish advisory are updated, they should encourage people to eat species with low mercury and high omega-3 levels. These documents should not only warn consumers about species with the highest mercury contamination but also identify those species that contain moderate amounts of mercury that can pose a risk for frequent seafood consumers.
Pregnant women and young children face greatest mercury risks
The 2010 Dietary Guidelines claimed that “moderate, consistent evidence shows that the health benefits from consuming a variety of seafood in the amounts recommended outweigh the health risks associated with methyl mercury” (USDA 2010). However, this assertion is dangerously out of step with the scientific evidence from dozens of observational studies. Even small exposures to mercury in the womb have been shown to inflict subtle but measurable deficits on children’s intelligence and nervous system.
Dozens of observational studies have shown that when pregnant women ingested food tainted with the particularly dangerous compound called methyl mercury, their children’s brain development was impaired, as measured by lower IQ scores and poorer outcomes on laboratory tests of memory, language skills and visual-motor function (Murata 2004, Debes 2006, Strain 2008, Karagas 2012). Mercury exposure during childhood is believed to cause similar deficits (Karagas 2012).
One of the most meticulous recent studies of American women, called Project Viva, examined 341 Boston-area women to determine the benefits and risks of seafood during pregnancy (Oken 2008). It found positive effects for children born to women who ate three or more seafood meals weekly but negative effects for the 10 percent of study participants with the highest mercury levels in their bloodstream. Frequent fish eating boosted children’s IQ measurements by about two to six points, but high mercury exposure during pregnancy dropped IQ scores by two to six points. An individual’s slight IQ deficit might seem subtle, but the social and economic toll on millions of children can be massive. Philippe Grandjean of Harvard University has estimated that American children lose 264,000 IQ points annually to mercury toxicity (Grandjean 2012).
The findings from Project Viva mirrored several other recent studies examining the effects of trace mercury consumption on fetal brain development (Sagiv 2012, Lederman 2008). Collectively, these findings contradict claims that the benefits of fish eating outweigh all risks.
These and other studies suggest that the EPA’s “safe level” for mercury exposure, technically the “reference dose,” set in 2001, is far too lax. It assumed that a pregnant woman could safely consume one tenth of a microgram of methyl mercury a day for every kilogram of bodyweight without risk to the fetus. Since pregnancy is a critical window of development and the fetal brain is the most sensitive to mercury toxicity, the EPA believed that this intake level also would be safe for children and adults (EPA 2001, Rice 2003). But later studies of American pregnancies found signs of mercury damage in children whose mothers’ mercury exposures were considerably lower than the 2001 EPA safe level (Grandjean 2012, Zero Mercury 2012).
EPA is planning to reevaluate its safe mercury level, but that process is likely to take at least four years. Until then EWG is using the existing “safe” level as an imperfect benchmark for mercury toxicity, but we recognize that these calculations likely underestimate the number of seafood species that pose mercury risks.
Women who eat fish frequently have high blood-mercury levels
A 2012 EPA review of nationally representative biomonitoring data for 10,000 American women reported what appeared to be a victory for public health advocates: The blood mercury measurements in American women of reproductive age dropped dramatically after the year 2000, even though self-reported seafood consumption remained stable (EPA 2013). This finding suggested that informed consumers may be taking to heart the warnings by state and federal agencies to eat fish but avoid high-mercury species.
However, on closer inspection, the study was not all good news. Its data suggest that women who eat seafood frequently still face a mercury problem. In the most recent survey period (2009-2010), the most frequent fish consumers reported eating six or more seafood meals per monthly, close to the Dietary Guidelines’ recommendation of eight meals a month. This group had the highest blood mercury concentrations of all; more than 10 percent of the women had mercury levels above the target concentration of 3.5 micrograms per liter that was determined to protect a developing fetus from exceeding EPA’s safety level for methyl mercury (Mahaffey 2009).
Tuna is a risky choice
Americans eat more than 400 million pounds of canned imported tuna because it is affordable and can be stored for a long time. Canned tuna is the second most popular seafood in the U.S., after shrimp. An average American eats an average of 2.5 pounds of tuna every year (NOAA 2012). Albacore tuna, also called “white” tuna, contains significant amounts of omega-3s, but tests indicate that it also contains significant amounts of mercury. “Light” tuna is usually skipjack tuna but can also contain yellowfin tuna. Skipjack and yellowfin have lower mercury levels than albacore, but fewer omega-3s.
The FDA/EPA fish advisory issued in 2004 said that pregnant women should limit their consumption of albacore tuna to six ounces weekly. However, EWG calculates that if a pregnant woman of light or average weight ate that much, she would exceed the EPA safe level. Children who ate a child-sized serving once a week would also exceed it.
The FDA/EPA advisory described canned light tuna as a lower mercury species, but it is not without mercury risk. EWG calculates that an average-weight pregnant woman who eats eight ounces of light tuna would consume enough mercury to reach half of EPA’s safe level for the week – too much, according to many expert accounts. Children of any weight could not eat two child-size servings of light tuna over a week without exceeding EPA’s safe level. Since EPA’s safe level may be too high, small women and children should eat light tuna only rarely. Because the current guidance is misleading, the next version of the FDA/EPA advisory must be updated to reflect the mercury risk of light tuna for small women and children.
The long, troubled history of government efforts against mercury
Mercury is a global contaminant emitted primarily by coal-fired power plants and mining operations. Mercury in vapor form condenses and falls into waterways and oceans, where it is transformed by bacteria and zooplankton into methyl mercury, an organic compound that is more toxic than the elemental form of mercury or inorganic mercury compounds. This methyl mercury pollution concentrates in the marine food chain. As a result, mercury concentrations are highest in predatory fish that eat smaller fish. Methyl mercury is highly toxic to the human brain, kidney, liver, heart and nervous system.
In acute cases, fish contamination has reached tragic proportions. Most notoriously, in the 1950s and 1960s severe mercury pollution near the Japanese fishing village of Minamata caused thousands of birth defects, mental retardation and a crippling syndrome that came to be known as Minamata disease.
Since 2009, FDA and EPA scientists have been collaborating on a joint effort to modernize and improve their 2004 guidelines on seafood, mercury and omega-3s. But according to agency insiders, the project has bogged down in interagency disputes. All the reasons for the gridlock have not been made known, but this much is certain: The financial stakes are enormous for seafood vendors, especially the multi-billion-dollar tuna industry.
In 2010, as the FDA and EPA grappled behind closed doors, the USDA and HHS were working with a panel of outside scientific and medical experts to draft the 7th edition of the Dietary Guidelines for Americans, which attempt to convey a comprehensive federal government stance on all nutrition policy issues.
EWG’s analysis concludes that both the 2010 Dietary Guidelines and the 2004 EPA/FDA advisory are seriously flawed on three counts:
- The Dietary Guidelines encourage people to eat more fish and to limit consumption of a few high-mercury species but do not point out the longer list of “moderate mercury” species that would pose a mercury risk when eaten twice weekly. EWG has determined that 19 of the 35 species it reviewed would pose a mercury risk to children, and 10 could be a concern for pregnant women of average weight who eat two servings of seafood a week.
- The Dietary Guidelines must do more to alert consumers to major differences in the omega-3 content of various types of seafood. Only 14 of the 35 species contain enough omega-3s to meet the nutritional recommendation of 1,750 milligrams of omega-3s weekly, assuming an individual eats eight ounces of that species each week.
- If all Americans followed the advice of the Dietary Guidelines, seafood consumption could double or triple, exerting even more pressure on fisheries already stressed by over-fishing.
All told, the federal government’s stance on seafood, mercury and omega-3s lacks both the clarity and precision needed to guide consumers toward the healthiest choices. Glossing over critical differences among different types of seafood can mislead some people into eating too much high-mercury fish and risking serious illness. Others who consume species too low in omega-3s will fail to get the desired benefits.
The ultimate solution is for the American government and other nations to reduce the mercury pollution that accumulates in seafood. A new global treaty known as the Minamata Convention aims to reduce mercury emissions from coal-fired power plants and small-scale mining, the two sources of mercury that most directly contribute to mercury contamination of global fisheries. As ocean temperatures rise because of global warming, however, mercury accumulation in seafood is projected to intensify.
EWG’s recommendations:
- Federal seafood consumption guidelines must be updated and improved. American consumers urgently need better advice about seafood choices. To help them avoid excessive mercury and consume enough omega-3 fatty acids, federal nutritional guidelines must:
- Give clear, portion-based guidelines for people who face various levels of risk, such as pregnant women, children and adults with cardiac disease.
- Clearly identify thresholds beyond which increased seafood consumption is unlikely to provide additional health benefits.
- Highlight fish choices that are low in mercury, high in omega-3s and sustainably produced.
- Emphasize risky fish choices, such as the 19 species of seafood that children should not eat more than once a week.
- EPA should lower its “safe level” of mercury. A substantial body of evidence suggests that mercury does more potent damage to the developing brain than previously thought. Earlier studies did not account for beneficial omega-3 fatty acids in fish consumed by populations under study. EPA must reevaluate its 2001 safe level (technically, the reference dose) and account for new information about mercury accumulation in the fetus and long-lasting intellectual impairment caused by trace mercury consumption. Public health agencies should update mercury safe limits for adults who are not pregnant, nursing or considering pregnancy.
- The federal government must improve its data collection for mercury and omega-3 fatty acid levels in fish. Clear, science-based guidance depends on robust data. A complicating factor in the nutritional guidelines for seafood ingestion is the high variability in seafood of omega-3 fatty acids, mercury and other contaminants. Mercury and omega-3 levels fluctuate within a single species depending on the age of the fish, fat concentrations, food source, season and region where caught. Both FDA monitoring for mercury levels and USDA evaluation of omega-3 fatty acid concentrations should be expanded to collect more samples.
- Mercury – Independent reviews have noted that FDA’s mercury monitoring program is incomplete and underestimates the true mercury levels for many species of seafood sold in the U.S. FDA must increase its monitoring to ensure that its recommendations accurately reflect real-world mercury exposures.
- Omega-3s – USDA’s nutrient database estimates for fish and shellfish are based on very few samples and may not reflect real-world exposures. USDA should increase the number of seafood samples it analyzes for its National Nutrient Database.
The federal government must investigate non-seafood sources of omega-3 fatty acids and provide consumers with better advice. The oceans do not produce enough seafood to accommodate the planet’s growing population and need for healthy omega-3 fats. The U.S. government should investigate alternative foods and supplements that could provide these vital fatty acids from safe and sustainable sources.


